“
“Keeping Everyone Safe in the Cath Lab”
– Robert F. Riley, MD, MS
Both the prevalence and complexity of coronary artery disease (CAD) are on the rise in the United States.¹ Although the terms “complex percutaneous coronary intervention (PCI)” and/or “CHIP” (complex, high-risk, and indicated PCI) remain somewhat ambiguous, various definitions exist, including anatomic/physiologic criteria (SYNTAX, SYNTAX II). There are also designations for these terms that include procedures with elevated periprocedural mortality risk compared to “routine PCI,” such as left main PCI (1%), chronic total occlusion (CTO) PCI (0.9%), lesions with significant calcification that require atherectomy (2.3%), device-assisted PCI (7.6%), PCI in patients turned down for coronary artery bypass grafting surgery (7.0%), and PCI in patients aged ≥ 80 years (3.2%).²⁻⁸ Regardless of how it is defined, interventional cardiologists are being increasingly asked to perform complex PCI in contemporary catheterization laboratories, and this is reflected in the direct relationship between CAD complexity and appropriateness for revascularization in societal guidelines and appropriate use criteria for PCI.⁹⁻¹⁰ This has led to a resurgence in novel techniques, devices, and data in order to meet this need.
Although the ability of PCI to treat anatomically complex CAD within high-risk patient subsets has significantly improved over the past 2 decades, coronary artery calcification represents a major challenge associated with adverse outcomes during and after PCI.¹¹⁻¹² Treatment with PCI in this patient group remains difficult due to a number of anatomic and technical factors, including reduced vessel compliance prohibiting stent delivery and reduced ability of implanted stents to expand and appose as required, both potentially culminating in a nidus for stent failure through either restenosis or stent thrombosis.¹³ Despite the use of high-pressure noncompliant (NC) balloons, cutting/scoring balloons, and atherectomy technologies to modify calcium, PCI of heavily calcified lesions is associated with an increased risk for early complications (dissection, perforation, and myocardial infarction) and/or late adverse events (restenosis, stent fracture, thrombosis, and repeat revascularization).¹⁴⁻¹⁷
ENSURING HIGH STANDARDS IN CALCIUM MODIFICATION IN COMPLEX PCI WHILE PRIORITIZING RADIATION SAFETY
In response to the unmet need for safe, reliable calcium modification for PCI, intravascular lithotripsy (IVL) has emerged as a novel therapy for the treatment of vascular calcification. IVL is based on the strategy of using acoustic pressure waves to treat renal calculi, with specific modifications in delivery to address vascular calcium. These adaptations include incorporating lithotripsy emitters on the shaft of a balloon angioplasty catheter that deliver localized, pulsatile, acoustic pressure waves circumferentially to modify vascular calcium.¹⁸ The safety and effectiveness of IVL have been reported across multiple clinical studies involving severely calcified CAD, particularly when compared to historical rates of adverse events with other types of calcium modification.¹⁹⁻²⁰
In addition to increased patient-level safety issues during complex PCI, there is also increased risk to the catheterization lab team during these procedures due to increased procedural times and radiation exposure, necessitating prolonged use of wearable lead aprons. Scatter radiation exposure for cath lab personnel has been associated with a threefold increase in the incidence of various cancers and a sixfold increase in the incidence of cataracts.²¹⁻²⁴ These risks have become increasingly apparent despite the use of standard radiation shielding in the room. With the increasing complexity of catheter-based interventions and subsequent cumulated radiation exposure over an entire career, the importance of radiation safety for health care workers has become paramount.
In addition to table- and ceiling-mounted lead shields, wearable apron shields are commonly utilized as radiation barriers in the cath lab and can remove between 80% and 97% of the incident radiation, depending on the “lead equivalency” of the shield.²⁵ However, aprons do not cover the head, neck, arms, lateral breast, or lower legs, leaving these areas exposed to substantial scatter radiation. In addition to their imperfect radiation protection, they also result in significant orthopedic injuries with longitudinal use, with over half of interventional cardiologists reporting at least one major orthopedic injury during their career.²⁶
EggNest Complete Radiation Protection System
The EggNest Complete Radiation Protection System (Egg Medical) is a novel radiation protection system that consists of a carbon fiber–based platform that is mounted onto the x-ray table (Figure 1). Flexible shielding (0.5-mm lead equivalence) below the table is affixed to the platform such that there is a radiation shield around the sides and head of the table that moves with the C-arm gantry. In addition, flip shields (0.5-mm lead equivalence) around the table can be rotated upwards after the patient is moved to the x-ray table to provide shielding around the patient that does not interfere with procedural performance.
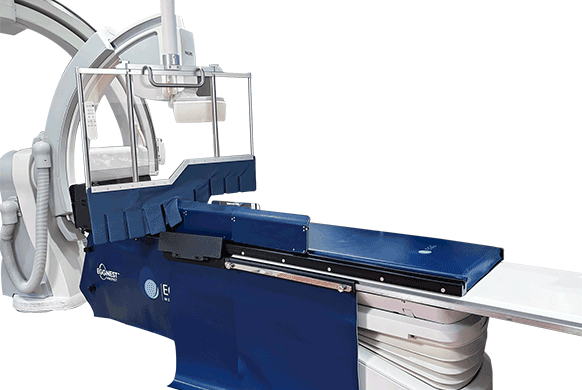
Figure 1. EggNest Complete Radiation Protection System.
A ceiling- or boom-mounted clear acrylic shield (the Complete Shield) with 1-mm lead-equivalent shielding is placed over the patient, such that a cutout with a radiation-shielding fringe is placed against the patient and extends across the arm. The right arm is held in a cradle with additional radiation shielding. A recent study showed that, compared to standard shielding, the EggNest Complete system significantly reduced radiation levels at all positions around the x-ray table. At the operator and assistant positions, EggNest Complete provided 98% reduction in scatter radiation dose.²⁷
Additionally, when compared to another novel radiation protection system, Rampart (Rampart IC), the EggNest Complete system provided additional significant protection for the head of the bed and the nurse positions, illustrating how the EggNest Complete system provided substantial reduction in scatter radiation exposure to all staff member positions in the room without increasing their risk for orthopedic injury.²⁸
